general medicine case presentation
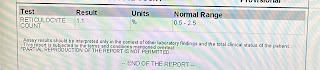
40 yr old male patient who is daily wage labourer by occupation came to OPD with Chief complaint of pain abdomen since 5 days associated with fever since 2 days HOPI Patient was apparently asymptomatic 5 days ago then he developed pain which is insidious in onset and gradually progressive which is diffuse , squeezing type and radiating to back . Pain is relieved on medication . No C/O of vomitings , loose stools , burning micturition ,cough,cold , chest pain , SOB Past history:- N/K/C/O TB , hypertension, diabetes, Asthma, epilepsy , CAD, thyroid disorders . Personal hisrory:- Diet - mixed Appetite- normal Bowel and bladder -regular Sleep - adequate Addictions - regular alcohol intake of 250 ml per day since 20 yrs . No food allergies and drug allergies General examination:- Pallor - yes Edema -absent Clubbing - absent Lymphadenopathy - absent Icterus - absent Cyanosis absent Vitals:- Temperature - 100.1F...
























Comments
Post a Comment