Case discussion
B.VAISHNAVI
3RD SEMESTER
ROLL NO. 22
This is an online E log platform to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. I have been given this case in order to solve in an attempt to understand the topic of patient's clinical data analysis to develop my competency in reading and comprehending clinical data and come up with a diagnosis and treatment plan.
A 45 year old female farmer by occupation presented with chief complaints of abdominal pain and vomiting since 4 days, headache since 1 day.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 5 days back. On Wednesday around 7:30 pm, pt alleged to be bitten by snake on right foot went to the local hospital, she is fine for 1 day. Had swelling of right lower limb, went to the local hospital ( ointment given)swelling subsided. Complained of vomiting(2-3 episodes), bilious ( food as content) since 4 days. Pt complained of abdominal pain since 4 days, squeezing type, in the periumbilical region, aggregated with vomiting, no radiation. Abdominal distension following food consumption.
Headache since 1 day
No photophobia, phonophobia, lacrimation, diplopia
No complaints of chest pain, palpitations
No complaints of SOB, PND
No complaints of burning micturition
No complaints of pedal edema, puffiness of face
HISTORY OF PAST ILLNESS:
No h/o of similar complaints in the past
N/K/C/O DM, Hypertension, epilepsy, TB
PERSONAL HISTORY:
Appetite normal
Mixed diet
Bowel movements- constipation
Bladder movements- normal
No addiction
FAMILY HISTORY:
Not significant
DRUG HISTORY:
No known allergies
GENERAL EXAMINATION:
Patient is conscious, coherent, coorperative
Moderately built and moderately nourished
Pallor present
No icterus
No cyanosis
No clubbing
No lymphadenopathy
No edema
VITALS:
Temperature: afebrile
PR:96 bpm
RR: 24 cpm
BP : 150/90 mm Hg
SPO2: 99%
GRBS: 180mg%
SYSTEMIC EXAMINATION:
CVS:
S1, S2 Heard
No thrills
No murmurs
RESPIRATORY SYSTEM:
Vesicular breath sounds heard
No dyspnoea
no wheeze sounds heard
ABDOMEN:
shape - scaphoid
Tenderness present in the periumbilical region
No palpable mass
Hernial orifices are normal
Free fluid absent
Liver and spleen - not palpable
Bowel sounds heard
CNS:
Pt is conscious, coherent, coorperative
Speech -normal
No signs of meningeal irritation
No abnormality detected
INVESTIGATIONS:
ELECTROCARDIOGRAM:
COMPLETE BLOOD PICTURE:
Hb- 8.5 gm%
RBC - 3.3 m/ cu mm
WBC- 9000/ cu mm
Platelets- 63,000/ cu mm
Neutrophils- 66%
Lymphocytes- 30%
Eosinophils- 02 %
Monocytes- 02%
Basophils- 00%
RANDOM BLOOD SUGAR :113 mg/dl
SERUM CREATININE: 1.4 mg/dl
SERUM URIC ACID : 7.2 mg/dl
BLEEDING TIME- 2 min 15 sec
CLOTTING TIME- 4 min 45 sec
LIVER FUNCTION TEST:
Total bilirubin- 1.0 mg/dl
Direct bilirubin- 0.2 mg/dl
Indirect bilirubin- 0.8 mg/dl
ALP- 90 IU/L
Total proteins- 6.7 gm
Albumin- 4.5 gm
Globulin- 2.2 gm
SGPT- 34 IU/L
SGOT- 24 IU/L
SERUM ELECTROLYTES:
BLOOD UREA:
URINE SODIUM:
URINE PROTEIN/ CREATININE RATIO:
RENAL FUNCTION TEST:
06/08/2021
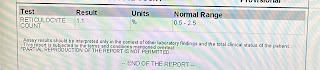
HEMOGRAM:
PROVISIONAL DIAGNOSIS:
ACUTE KIDNEY INJURY SECONDARY TO ACUTE TUBULAR NECROSIS, SNAKE BITE? TOXINEMIA.
TREATMENT:
Rx:
IVF 20 NS, 20RL @ 100 ML/DAY
INJ PAN 40 MG IV/OD
INJ ZOFFER 4MG/IV/TID
INJ BUSCOPAN IM/BD
BP/PR/RR/SPO2 - 4TH HRLY
GRBS CHARTING -6TH HRLY
STRICT I/O CHARTING
TAB PCM 650 MG PO/SOS
INJ LASIX 40 MG IV/BD
IF SBP>=100 mmHg
















Comments
Post a Comment