GENERAL MEDICINE CASE DISCUSSION
B.VAISHNAVI
3RD SEMESTER
ROLL NO. 22
This is an online E log platform to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. I have been given this case in order to solve in an attempt to understand the topic of patient's clinical data analysis to develop my competency in reading and comprehending clinical data and come up with a diagnosis and treatment plan.
Under the guidance of Dr. SREEJA (intern)
A CASE OF CHRONIC LIVER DISEASE SECONDARY TO ALCOHOLISM
A 43 year old male laborer by occupation presented with chief complaints of pedal edema since 30 days, abdominal distension since 15 days.
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 30 days back, had history of onset of swelling in the bilateral lower limbs, insidious, gradually progressive bilaterally up to the knee, pitting type, tender since 30 days, abdominal distension-progressive since 15 days, and not associated with facial puffiness, fatigue.
No h/o of fever, pain abdomen, nausea, vomiting, SOB, palpitations.
HISTORY OF PAST ILLNESS:
No h/o of similar complaints in the past
K/C/O DM II since 5 years(on medication for 2 years, later stopped)
N/K/C/O Epilepsy, Hypertension, TB
PERSONAL HISTORY
Mixed diet
Appetite normal
Sleep adequate
Bowel and Bladder movements regular
Addiction- Consumption of liquor since 18 years (180 ml)
Tobacco chewing:1-2/day since 15 years
FAMILY HISTORY:
Not significant
DRUG HISTORY:
On medication for DM II since one month
No known allergies
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative
Moderately built and Moderately nourished
No Pallor
No Cyanosis
No Clubbing
No Icterus
No Generalized lymphadenopathy
Pedal edema-Bilateral, pitting type up to the knee
VITALS
Temperature: Afebrile
PR: 74 bpm
RR: 16 cpm
BP: 110/60 mm of Hg
SPO2: 98%
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
S1, S2 heard
No murmurs
RESPIRATORY SYSTEM:
BAE+
NVBS heard
CENTRAL NERVOUS SYSTEM:
Intact
No focal defect
No abnormality detected
ABDOMEN:
Distended abdomen
Scar is present in the centre
Umbilicus everted
Hernial orifices normal
Visible veins present
No visible pulsations
Palpitation:
Tenderness+
No local rise in temperature
Inspectory findings are confiirmed
No palpable mass
Liver, spleen not palpable
Free fluid present
Fluid thrills absent
Percussion:
Shifting dullness present
Auscultation:
Bowel sounds heard
INVESTIGATIONS:
24/07/2021
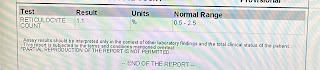
HEMOGRAM:
LIVER FUNCTION TEST:
SERUM ELECTROLYTES:
SERUM CREATININE:
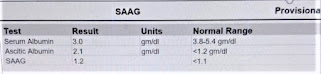
ASCITIC FLUID PROTEIN SUGAR:
ASCITIC FLUID FOR LDH:
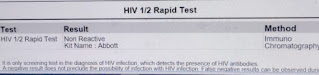
HIV 1/2 RAPID TEST:
ANTI HCV ANTIBODIES-RAPID:
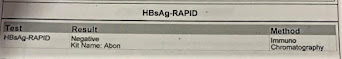
HBsAg -RAPID:
26/07/2021
25/07/2021
No fresh complaints, stools passed
O/E, pt is c/c/c
afebrile
PR 74 bpm
BP 110/60 mm Hg
RR 16 cpm
SPO2 98% on room air
GRBS 151 mg/dl
CVS: S1 S2 heard
RS: NVBS +
P/A DISTENDED, FREE FLUID+, FLUID THRILL+
Rx:
FLUID RESTRICTION <1L/DAY
INJ THIAMINE 1AMP IN 100ML NS IV/BD
INJ OPTINEURON 1AMP IN 100ML NS IV/OD
T. LASILACTONE (40/100) PO/OD
T. RIFAXIMIN 550 MG PO/OD
SYP LACTULOSE 15 ML PO/OD TO PASS [STOOLS <= 2/DAY]
ABDOMEN GIRTH AND WEIGHT MONITORING -DAILY
BP/PR/TEMP/RR- 4TH HRLY
GRBS- 6TH HRLY
INFORM GRBS
INJ HAI S/C ACC TO SLIDING SCALE
8AM - 2PM - 8PM
26/07/2021
No fresh complaints, stools passed
Appetite improved
O/E, pt is c/c/c
Afebrile
PR - 72bpm
BP- 110/60
RR- 16 cpm
CVS: S1 S2 heard
CNS: No abnormality detected
RS: NVBS+
P/A: DISTENDED, FREE FLUID+, FLUID THRILLS ABSENT
Rx:
FLUID RESTRICTION<1L/ DAY
SALT RESTRICTION<2.4GR/ DAY
INJ THIAMINE 1 AMP IN 100 ML NS IV/TID
INJ OPTINEURON 1 AMP IN 100 ML NS IV/ OD
T. LASILACTONE(40/100) PO/OD
T. RIFAXIMIN 550 MG PO/BD
ABDOMINAL GIRTH MONITOR DAILY
WEIGHT MONITORING DAILY
BP/ PR/ TEMP/ Rx- 12 TH HRLY
GRBS- 6 TH HRLY
HAI S/C ACC TO SLIDING SCALE
8 AM - 3 PM - 8PM
T. LIVOGEN 150 MG PO/OD
I/O CHARTING
27/07/2021
No fresh complaints, stools passed
Appetite improved
O/E pt is c/c/c
Afebrile
PR- 76 bpm
BP- 110/60 mm Hg
RR- 14 cpm
CVS: S1 S2 heard, no murmers
CNS: no abnormality detected
RS: NVBS +
P/A: DISTENDED, FREE FLUID +, FLUID THRILLS ABSENT
FLUID RESTRICTION < 1L/DAY
SALT RESTRICTION< 2.4 GR/ DAY
INJ THIAMINE 1 AMP IN 100 ML NS IV/TID
INJ OPTINEURON 1 AMP IN 100 ML NS IV/OD
T. LASILACTONE (40/100) PO/OD
T. RIFAXIMIN 550 MG PO/BD
ABDOMINAL GIRTH MONITOR DAILY
WEIGHT MONITORING DAILY
BP/PR/TEMP/Rx -12 HRLY
GRBS - 6TH HRLY
HAI S/C ACC TO SLIDING SCALE
8AM - 3PM- 8PM
T. LIVOGEN 150 MG PO/OD
I/O CHARTING
DEPARTMENT OF GENERAL MEDICINE DISCHARGE SUMMARY:
IPID: 202116709
Age/ Gender: 43 years/ Male
Admission date : 24/07/2021
Discharge date: 27/07/2021
Ward: AMC
Unit: VI
NAME OF TREATING FACULTY:
DR. NUTHNA SRIYA ( INTERN)
DR. SREEJA ( INTERN)
DR. KEERTHI REDDY ( INTERN)
DR. SANGEETHA ( NTERN)
DR. MANASA (PGY1)
DR. ZAIN ALAM (PGY2)
DR. AJITH (PGY2)
DR. ARJUN KUMAR (AP)
DR. RAKESH BISWAS (HOD)
Diagnosis: CHRONIC LIVER DISEASE SECONDARY TO ALCOHOLISM
Case history and clinical findings:
A 43 YEAR OLD MALE LABORER BY OCCUPATION PRESENTED WITH CHIEF COMPLAINTS OF PEDAL EDEMA SINCE 30 DAYS, ABDOMINAL DISTENSION SINCE 15 DAYS
HISTORY OF PRESENTING ILLNESS:
THE PATIENT WAS APPARENTLY ASYMPTOMATIC 30 DAYS BACK, HAD HISTORY OF ONSET OF SWELLING IN THE BILATERAL LOWER LIMBS, INSIDOUS, GRADUALLY PROGRESSIVE UPTO THE KNEE, PITTING TYPE, TENDER SINCE 30 DAYS, ABDOMINAL DISTENSION-PROGRESSIVE SINCE 15 DAYS, NOT ASSOCIATED WITH FACIAL PUFFINESS, FATIGUE.
NO H/O FEVER, PAIN ABDOMEN, NAUSEA, VOMITING, SOB, PALPITATIONS
HISTORY OF PAST ILLNESS
NO H/O OF SIMILAR COMPLAINTS IN THE PAST
K/C/O DM II SINCE 5 YEARS( ON MEDCATION FOR 2 YEARS, LATER STOPPED)
N/K/C/O EPILEPSY, HYPERTENSION, TB
PERSONAL HISTORY:
MIXED DIET
APPETITE NORMAL
SLEEP ADEQUATE
BOWEL AND BLADDER MOVEMENTS REGULAR
ADDICTON- CONSUMPTION OF LIQUOR SINCE 18 YEARS( 180 ML)
TOBACCO CHEWING- 1-2/DAY SINCE 15 YEARS
FAMILY HSTORY:
NOT SGNIFICANT
DRUG HISTORY:
ON MEDCATION FOR DM II SINCE ONE MONTH
NO KNOWN ALLERGIES
GENERAL EXAMINATION:
PATIENT IS CONSCIOUS, COHERENT, COOPERATIVE
MODERATELY BUILT AND MODERATELY NOURISHED
NO PALLOR
NO CYANOSIS
NO CLUBBING
NO ICTERUS
NO GENERALIZED LYMPHADENOPATHY
PEDAL EDEMA- BILATERAL, PITTING TYPE UP TO THE KNEE
VITALS:
TEMPERATURE- AFEBRILE
PR- 74 bpm
RR- 16 cpm
BP- 110/60 mm Hg
SPO2- 98%
SYSTEMIC EXAMINATION:
CVS:
S1, S2 HEARD
NO MURMERS
RESPIRATORY SYSTEM :
BAE+
NVBS HEARD
CNS:
INTACT
NO FOCAL DEFECT
NO ABNORMALITY DETECTED
ABDOMEN:
DISTENDED ABDOMEN
SCAR IS PRESENT IN THE CENTRE
UMBILICUS EVERTED
HERNIAL ORIFICES NORMAL
VISIBLE VEINS +
NO VISIBLE PULSATIONS
PALPATION:
TENDERNESS+
NO LOCAL RISE IN TEMPERATURE
INSPECTORY FINDINGS ARE CONFIRMED
NO PALPABLE MASS
LIVER, SPLEEN NOT PALPABLE
FREE FLUID +
FLUID THRILLS ABSENT
PERCUSSION:
SHIFTING DULLNESS +
AUSCULTATION:
BOWEL SOUNDS HEARD
INVESTIGATIONS:
ECG; NORMAL SINUS RHYTHM
ULTRASOUND ABD- F/S/O CHRONIC LIVER DISEASE, GROSS ASCITES, RAISED ECHOGENECITY OF B/L KIDNEYS CORRELATE WITH RFT, RIGHT SIMPLE RENAL CYST
ENDOSCOPY: LOW GRADE OESOPHAGEAL VARICES AND SEVERE PHG
COMPLETE URINE EXAMINATION ( CUE) 24/07/2021 11:47 AM
COLOUR- PALE YELLOW
APPEARANCE- CLEAR
REACTION- ACIDIC
SP. GRAVITY- 1.010
ALBUMIN- NIL
SUGAR- NIL
BILE SALTS-NIL
BILE PIGMENTS- NIL
PUS CELLS- 2-3
EPITHELIAL CELLS- 2-3
RED BLOOD CELLS- NIL
CRYSTALS- NIL
CASTS- NIL
AMORPHOUS DEPOSITS- ABSENT
OTHERS- NIL
SERUM ELECTROLYTES (Na, K, Cl) 24/07/2021 11:47 AM
SODIUM - 135 mEq/L ( 136- 145 mEq/L )
POTASSIUM - 4.1 mEq/L (3.5 - 5.1 mEq/L )
CHLORIDE - 101 mEq/L ( 98 - 107 mEq/L )
SERUM CREATININE 24/07/2021 11:47 AM
SERUM CREATININE- 0.8 mg/dl ( 0.9- 1.3 mg/dl )
LIVER FUNCTION TEST( LFT) 24/07/2021 11:47 AM
TOTAL BILIRUBIN- 0.62 mg/dl ( 0-1 mg/dl )
DIRECT BILIRUBIN - 0.20 mg/dl ( 0- 0.2 mg/dl)
SGOT(AST)- 23 IU/L (0-35 IU/L)
SGPT(ALT)- 18IU/L (0-45 IU/L)
ALKALINE PHOSPHATE- 160 IU/L ( 53-128 IU/L)
TOTAL PROTEINS- 6.3 gm/dl (6.4- 8.3 gm/dl)
ALBUMIN- 3.0 gm/dl (3.5- 5.2 gm/dl)
A/G RATIO-0.9
ANTI HCV ANTIBOBIES - RAPID- NON REACTIVE KIT
TREATMENT GIVEN( ENTER ONLY GENERIC NAME)
24/07/2021
INJ THIAMINE 1 AMP IN 100 ML NS/IV/OD
INJ OPTINEURON 1 AMP IN 100 ML NS IV/OD
T. LASILACTONE ( 40/100) PO/OD
FLUID RESTRICTION <1L/DAY
T. RIFAXIMIN 550 MG PO/OD
BP/PR/SPO2-MONITORING 2 ND HRLY
GRBS- 6TH HRLY
ABDOMINAL GIRTH MEASUREMENT DAILY
SYP LACTULOSE 15 ML/PO/OD
INJ HAI S/C ACC TO SLIDING SCALE
25/07/2021
FLUID RESTRICTION <1 L / DAY
INJ THIAMINE 1 AMP IN 100 MLNS IV/BD
INJ OPTNEURON 1 AMP IN 100ML NS IV/OD
T. LASILACTONE (40/100) PO/OD
T. RIFAXIMIN 550 MG PO/OD
SYP LACTULOSE 15 ML PO/OD TO PASS STOOLS ( <= 2/ DAY)
ABDOMEN GIRTH AND WEIGHT MONITORING-DAILY
BP/PR/TEMP/RR- 4TH HRLY
GRBS- 6TH HRLY
INFORM GRBS
INJ HAI S/C ACC TO SLIDING SCALE
8AM - 2PM - 8PM
26/07/2021
FLUID RESTRICTION < 1L/DAY
SALT RESTRICTION < 2.4 GR/DAY
INJ THIAMINE 1 AMP IN 100 ML NS IV/TID
INJ OPTINEURON 1 AMP IN 100 ML NS IV /OD
T. LASILACTONE( 40/100) PO/OD
T. RIFAXIMIN 550 MG PO/BD
ABDOMINAL GIRTH MONITOR DAILY
WEIGHT MONITORING DAILY
BP/ PR/ TEMP / Rx -12 TH HRLY
GRBS- 6TH HRLY
HAI S/C ACC TO SLIDING SCALE
8AM- 3PM-8PM
T. LIVOGEN 150 MG PO/OD
I/O CHARTING
27/07/2021
FLUID RESTRICTION < 1L/DAY
SALT RESTRICTION < 2.4 GR/DAY
INJ THIAMINE 1 AMP IN 100 ML NS IV/TID
INJ OPTINEURON 1 AMP IN 100 ML NS IV/OD
T.LASILACTONE ( 40/100) PO/OD
T.RIFAXIIMIN 550 MG PO/BD
ABDOMINAL GIRTH MONITORING DAILY
WEIGHT MONITORING DAILY
BP/PR/TEMP/Rx-12 TH HRLY
GRBS- 6TH HRLY
HAI S/C ACC TO SLIDING SCALE
8AM- 3PM- 8 PM
T. LIVOGEN 150 MG PO/OD
I/O CHARTING
ADVICE AT DISCHARGE:
FLUID RESTRICTION <1L/DAY
SALT RESTRICTION< 2.4 GR/DAY
TAB. THIAMINE 100 MG BD/PO FOR 15 DAYS
TAB. MVT OD/PO FOR 15 DAYS
TAB. GLIMI M1 PO/OD FOR 15 DAYS
T. LASILACTONE ( 40/100) PO/OD FOR 7 DAYS
T. RIFAXIMIN 550 MG PO/BD
T.LIVOGEN 150 MG PO/OD FOR 15 DAYS
PROTEIN RICH FOOD, STRICT DIABETIC DIET
FOLLOW UP:
REVIEW AFTER 15 DAYS TO MEDICINE OP WITH FBS AND PLBS
WHEN TO OBTAIN URGENT CARE
IN CASE OF ANY EMERGENCY IMMEDATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT
PREVENTIVE CARE:
AVO SELF MEDICATION WITHOUT DOCTORS ADVICE, DONOT MISS MEDICATIONS. IN CASE OF EMERGENCY OR TO SPEAK TO YOUR TREATING FACULTY OR FOR APPOINTMENTS, PLEASE CONTACT : 08682279999 FOR TREATMENT REQUIRES PATIENT/ ATTENDENT DECLARATION:- THE MEDICINES PRESCRIBED AND THE ADVICE REGARDING PREVENTIVE ASPECTS OF CARE, WHEN AND HOW TO OBTAIN URGENT CARE HAVE BEEN EXPLAINED TO ME IN MY OWN LANGUAGE
SIGNATURE OF PATIENT/ ATTENDER
SIGNATURE OF PG/ INTERN
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
.















Comments
Post a Comment